When it comes to bloodborne pathogens, the first and most important rule is simple: treat all human blood and certain bodily fluids as if they are infectious. This guiding principle, known as Universal Precautions, is the bedrock of safety in any environment where biological hazards may be present.
This is not about fear; it is about establishing a professional, non-negotiable standard of safety. It means understanding the science behind pathogen transmission, always using proper Personal Protective Equipment (PPE) as a barrier, and following decontamination protocols with methodical precision. For trained professionals, this mindset is second nature and the foundation of protecting ourselves, our teams, and the public.
Recognizing the Unseen Dangers of Bloodborne Pathogens
To effectively protect yourself, it is critical to understand the nature of the threat. Bloodborne pathogens are microscopic organisms in human blood that can cause serious, often lifelong, diseases. They are invisible, silent, and demand professional respect.
The most widely known pathogens include:
- Human Immunodeficiency Virus (HIV), which attacks and weakens the body's immune system.
- Hepatitis B Virus (HBV), a severe liver infection that can become a chronic, long-term illness.
- Hepatitis C Virus (HCV), another viral liver infection capable of causing significant, lasting health complications.
However, the list of potential threats is extensive. For a comprehensive overview, you can learn more about the most common bloodborne pathogens in our detailed guide.
What makes these pathogens particularly dangerous is their stealth and resilience. For instance, HBV can remain infectious in dried blood for a week or more. A seemingly old, innocuous stain can still pose a significant biological risk, which is why professional assessment is crucial.
Common Real-World Exposure Scenarios
Exposure risk is not confined to clinical settings. It can occur in any environment—an industrial site, a school, or a private residence following an accident.
Transmission typically happens through specific pathways:
- Punctures or Cuts: This includes needlestick injuries but also cuts from contaminated broken glass or other sharp objects.
- Contact with Mucous Membranes: A splash of blood or other potentially infectious material (OPIM) into the eyes, nose, or mouth.
- Contact with Non-Intact Skin: When infectious material comes into contact with skin compromised by a pre-existing cut, rash, or abrasion.
Understanding that many Sexually Transmitted Diseases (STDs) are also bloodborne reinforces the broad spectrum of risks and underscores why proper, professional-grade protection is critical.
The Critical Need for a Proactive Mindset
The data on occupational exposure is sobering. Globally, an estimated 3 million healthcare workers are exposed to bloodborne pathogens like HIV, HBV, and HCV annually.
These exposures lead to approximately 66,000 hepatitis B infections, 16,000 hepatitis C cases, and up to 5,000 HIV infections each year. Alarmingly, over 90% of these incidents occur in low-income countries, highlighting the vital importance of proper training, resources, and strict adherence to safety protocols.
This data reinforces a fundamental truth in the biohazard remediation industry: prevention is everything. A single moment of complacency or a failure to use the correct equipment can have life-altering consequences.
This is precisely why the field of professional biohazard remediation exists. Our work is not merely "cleaning up"; it is the methodical elimination of an invisible threat using scientific principles, strict regulatory compliance, and an unwavering commitment to safety. Every protocol we follow—from selecting a specific respirator to establishing complex decontamination zones—is designed to break the chain of infection and restore a space to a state of biological safety. This proactive, compliance-driven mindset is what distinguishes a professional remediation expert from a standard cleaning service and is core to how we protect our clients and communities.
Your First Line of Defense: PPE and Smart Controls
Knowing the risks is the first step, but actively mitigating them is what ensures safety. When facing potential biohazards, safety depends on creating robust barriers between you and the threat. This is achieved through a combination of Personal Protective Equipment (PPE) and environmental modifications known as engineering and administrative controls.
Viewing PPE as mere "equipment" is a common but dangerous misconception. It is a complete system, with each component designed to protect against specific routes of infection. The required level of PPE depends entirely on the situation. A minor, contained spill on a non-porous surface may only require gloves, while a complex trauma scene demands a full-body, fluid-resistant suit, a respirator, and a heightened level of procedural discipline.
This flowchart illustrates the critical chain of events that can lead to an infection and highlights where protective measures must intervene.
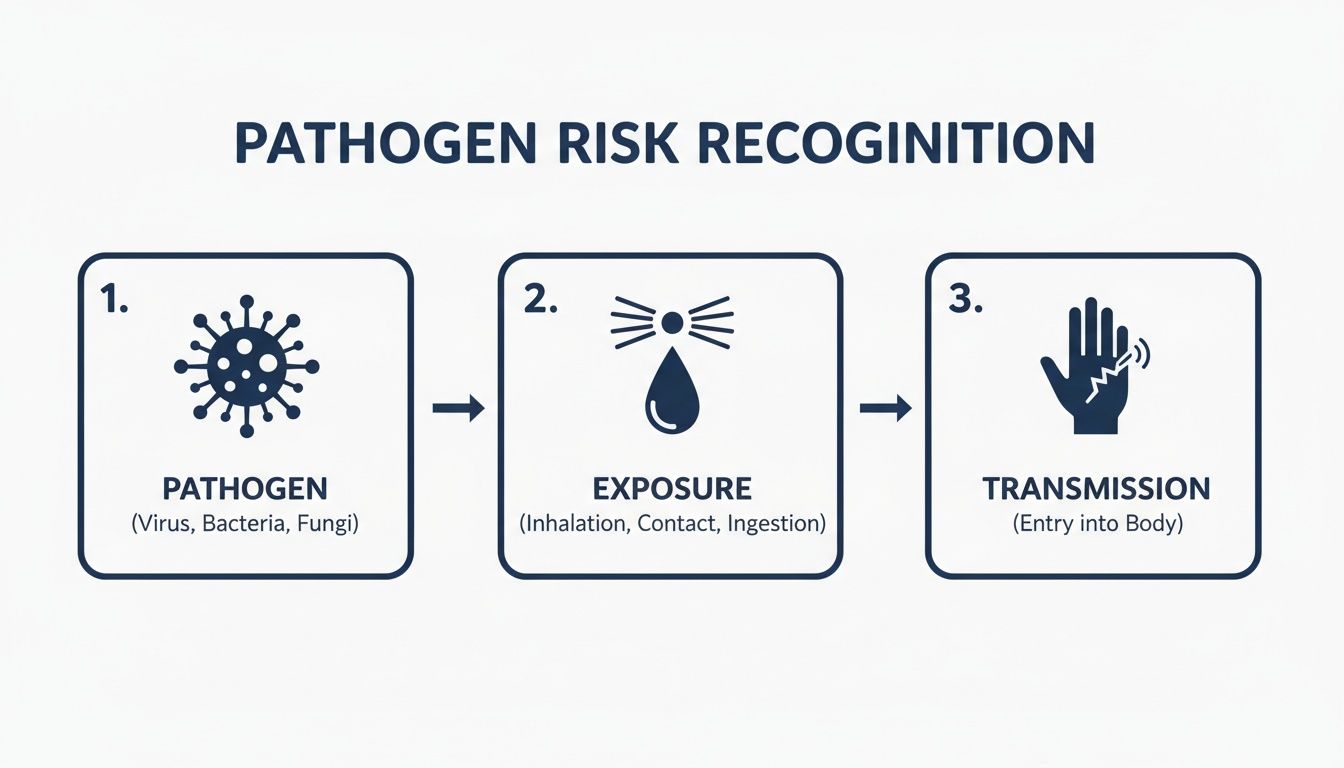
As shown, for an infection to occur, a pathogen requires a pathway to an entry point. PPE and other controls are engineered to break this chain at the point of exposure, effectively stopping the pathogen.
Selecting The Right Personal Protective Equipment
Choosing the correct PPE is the most critical initial step in any situation involving potential exposure. Each piece serves a specific function, and understanding this is key to building an effective protective barrier.
The table below outlines the essential equipment used by biohazard remediation professionals. It serves as a foundational guide for appropriate gear selection, from minor incidents to high-risk scenes.
| PPE Component | Primary Function | When It Is Required | Key Selection Tip |
|---|---|---|---|
| Gloves | Protects hands from direct contact with blood and OPIM. | Any time there is a risk of touching contaminated surfaces. | Always use medical-grade nitrile or vinyl gloves. Double-gloving is a best practice for tasks with a high tear risk. |
| Gown/Coveralls | Shields skin and clothing from splashes, splatters, and saturation. | When splashes are likely or for large-scale contamination. | Choose a fluid-resistant gown for moderate risk; full-body impermeable coveralls for high risk. |
| Eye/Face Protection | Prevents pathogens from entering through mucous membranes (eyes, nose, mouth). | Any task that could generate splashes or aerosols. | Goggles provide a seal for minimum protection. A full-face shield is superior for significant splash potential. |
| Mask/Respirator | Filters airborne droplets and particles from the air you breathe. | When airborne particles or strong odors are present. | A surgical mask blocks droplets. A fit-tested N95 respirator is required for airborne contaminants. |
Acquiring the right gear is only the beginning. For a deeper understanding of how each component integrates into a comprehensive safety plan, explore our guide on the role of PPE in ensuring safety during biohazard cleanup. This is fundamental knowledge for any professional facing these occupational risks.
The Critical Art of Donning and Doffing
Possessing the best PPE is ineffective if you contaminate yourself while putting it on or—more commonly—taking it off. The procedures for donning (putting on) and doffing (taking off) are methodical and must be followed without deviation.
Cross-contamination during doffing is a leading cause of occupational exposures. It is a skill that requires training and practice.
The guiding principle is to remove the most contaminated items first while meticulously avoiding contact with your clean skin. For example, one glove is peeled off with the other gloved hand, and then a clean finger is slid under the cuff of the remaining glove to remove it safely.
Professional remediation teams practice these procedures rigorously. Every movement is deliberate, designed to contain the hazard on the exterior of the equipment and ensure the technician is completely free of contaminants once the gear is removed. This level of discipline is essential for ensuring safety in high-stress environments.
Engineering and Administrative Controls
While PPE is a personal shield, a truly safe environment relies on controls that remove the hazard or modify work practices. These controls are often more effective than PPE because they do not depend on individual behavior.
Engineering Controls are physical modifications to the work environment designed to isolate people from danger.
- Sharps Disposal Containers: Puncture-resistant, leak-proof containers are a simple yet highly effective way to prevent needlestick injuries.
- Splash Guards: Physical barriers in laboratory or medical settings are an effective measure for protecting workers from accidental splashes.
- Biohazard Bags: Using designated red bags for regulated medical waste clearly communicates that the contents require specialized handling, preventing accidental exposure.
Administrative Controls are policies and procedures implemented to reduce exposure risk.
- Decontamination Zones: We establish "hot," "warm," and "cold" zones at every remediation site. This structured approach controls the movement of personnel and equipment, preventing contaminants from being tracked out of the affected area.
- Mandatory Training: Regular, hands-on training is not a suggestion; it is an OSHA requirement and a cornerstone of our safety culture. It ensures every team member can protect themselves and others.
- No Eating or Drinking: A strict policy prohibiting food, drink, or smoking in work areas eliminates a significant and avoidable route of exposure.
By layering appropriate PPE with intelligent engineering and administrative controls, a comprehensive defense system is created. This multi-faceted strategy is the hallmark of professional biohazard remediation and the only reliable method to guarantee safety.
Implementing Proactive Safety Measures and Training
While physical barriers are essential, true protection is proactive. It involves building systems and habits that prevent exposure incidents from occurring. Central to this strategy is one of modern medicine's most powerful tools against a major bloodborne threat.
The Hepatitis B vaccine is the single most effective defense against HBV infection. For anyone in a high-risk profession—from healthcare and emergency response to our work in biohazard remediation—vaccination is a non-negotiable layer of personal protection. It drastically reduces the risk of contracting this resilient and potentially chronic liver disease.
The Power of Immunization
The impact of vaccination is significant. An unvaccinated individual who sustains a needlestick from an HBV-positive source faces up to a 30% risk of infection. For a vaccinated individual, that risk drops to less than 5%.
Unfortunately, there is a concerning trend of falling Hepatitis B vaccination rates among at-risk groups. This decline in immunity directly increases exposure risks. If your occupation involves potential exposure, confirming your vaccination status is a critical component of personal risk management.
Establishing a Formal Exposure Control Plan
A culture of safety is built not on intentions, but on a clear, written plan. This is where the Occupational Safety and Health Administration (OSHA) provides a framework. OSHA mandates that any workplace with potential occupational exposure to bloodborne pathogens must develop and implement a formal Exposure Control Plan (ECP). This document serves as the operational playbook for safety.
A robust ECP is a living document, reviewed annually and updated whenever new tasks or procedures alter exposure risks.
Its core components include:
- Exposure Determination: Identifying which job roles and specific tasks could reasonably result in contact with blood or OPIM.
- Methods of Compliance: Detailing the specific engineering controls, work practice controls, and PPE that will be used to eliminate or minimize exposure.
- Hepatitis B Vaccination Program: Outlining how the employer will offer the HBV vaccine series, free of charge, to all employees with occupational exposure.
- Post-Exposure Evaluation and Follow-up: A critical section that defines the exact steps to take following an exposure incident, from reporting to confidential medical evaluation.
- Communication of Hazards: Describing the use of labels, signs (like the universal biohazard symbol), and information to ensure all personnel are aware of the risks.
An ECP is far more than a compliance document—it is a tangible commitment to the health and safety of your team. It translates abstract regulations into concrete, actionable steps, eliminating guesswork in high-stress situations and forming the foundation of a safe work environment.
Beyond PPE, proactive safety means implementing thorough environmental controls, which include robust commercial disinfection and sanitizing practices.
The Non-Negotiable Role of Regular Training
An ECP is only effective if the team follows it. This is why regular, high-quality training is indispensable. Safety is a skill that requires practice and continuous reinforcement to maintain proficiency.
Effective training is interactive and tailored to the real-world tasks employees perform. This includes hands-on drills for donning and doffing PPE, mock spill cleanups, and role-playing the post-exposure reporting process.
Annual refresher training is more than an OSHA requirement; it is a practical necessity. It keeps protocols current, introduces new best practices, and reinforces the muscle memory needed to act correctly and calmly during an emergency. You can dive deeper into the crucial role of training in biohazard cleanup in our article.
Ultimately, consistent training fosters a culture where safety is a shared responsibility, protecting everyone from the technician on-site to the clients and communities we serve.
What to Do Immediately After an Exposure Incident

Even with the best training and procedures, accidents can happen. In such an event, a calm, methodical response is your greatest asset. Knowing the precise steps to take after a potential exposure is as vital as the preventive measures themselves. The actions taken in the first few minutes and hours can dramatically reduce the risk of infection.
First Aid: The First Critical Seconds
The moments immediately following an exposure are the most critical window for intervention. The appropriate first aid response depends on the nature of the contact and must be performed without delay.
- For Needlesticks or Cuts: Immediately wash the wound with soap and running water. Allow the wound to bleed freely but gently; never squeeze or scrub it, as this can cause further tissue damage and potentially push contaminants deeper.
- For Splashes to Skin: If blood or OPIM contacts skin with existing cuts, rashes, or abrasions, wash the area thoroughly with soap and water immediately.
- For Splashes to Eyes, Nose, or Mouth: This is an emergency requiring immediate and prolonged flushing. Use an emergency eyewash station if available. Otherwise, flush the area with clean, running water or saline for at least 15 minutes.
These initial actions are designed to physically remove as much infectious material as possible before it can enter your system.
Reporting and Documentation: Your Next Steps
After administering immediate first aid, the incident must be officially reported and documented. This is a critical step for ensuring proper medical follow-up and legal protection.
Notify your designated supervisor or the individual responsible for your company's Exposure Control Plan immediately. Time is of the essence, and they must initiate the post-exposure protocol without delay.
Next, detailed documentation is required. This information is what medical professionals will use to assess your risk.
Record every detail: the date and time of the incident, the procedure being performed, the type and amount of fluid involved, and the exact mechanism of exposure. If the source individual is known, their identity should be confidentially documented. This precision is invaluable for the medical team's assessment.
This record is vital for any workers' compensation claims and ensures you receive the appropriate medical evaluation. For a deeper understanding of an employer's responsibilities, you can review the official OSHA guidelines for biohazard exposure and workplace incidents.
Seeking Immediate Medical Evaluation
Following the report, a confidential medical evaluation from a healthcare professional must be obtained as soon as possible. This is not a "wait and see" situation. This evaluation determines your true level of risk and the necessary course of action.
The process typically includes:
- Assessing the Exposure: The provider will review your report and ask detailed questions to understand the incident's severity.
- Evaluating the Source: If the source individual is known and provides consent, they will be tested for HIV, HBV, and HCV to determine the specific risk.
- Baseline Testing: Your blood will be drawn and tested to establish your baseline status for HIV, HBV, and HCV.
Your employer is required by law to provide this medical follow-up confidentially and at no cost to you. The most urgent consideration during this evaluation is the potential need for Post-Exposure Prophylaxis (PEP).
PEP is a course of antiretroviral medication taken shortly after a potential HIV exposure to prevent the virus from establishing an infection. For maximum efficacy, PEP must be started as soon as possible, ideally within hours. It is generally not recommended after 72 hours have passed. This narrow window underscores why every second counts. A rapid response provides the best opportunity to protect your long-term health.
Mastering Decontamination and Biohazard Waste Disposal
The remediation process is not complete once the visible contamination is removed. True safety is achieved through the final, critical steps: methodical decontamination and compliant waste disposal. Failing to execute these stages properly negates all previous safety efforts and can leave behind latent health risks and significant legal liability.

Decontamination is not simply wiping down a surface. It is a scientific process designed to eradicate pathogens, demanding the correct chemicals, strict procedural adherence, and a thorough understanding of microbiological threats.
The Science of an Effective Cleanup
To properly decontaminate a surface, professionals use disinfectants proven to kill the most resilient pathogens. This is why the industry standard is an EPA-registered, tuberculocidal disinfectant. The organism that causes tuberculosis is notoriously difficult to eliminate; therefore, a product effective against it can be trusted to neutralize a wide range of other viruses and bacteria, including HIV, HBV, and HCV.
The chemical agent is only one part of the equation. Contact time—the duration a disinfectant must remain wet on a surface to be effective—is equally critical. Wiping a surface dry prematurely can render the disinfectant useless. Each product has a specific, scientifically validated contact time, often several minutes, that must be strictly followed.
Navigating the Maze of Biohazard Waste Rules
Following remediation, you are left with regulated biohazardous waste. This material cannot be discarded in standard trash. A complex network of federal, state, and local regulations governs every aspect of its handling, from initial containment to final destruction. The penalties for non-compliance are severe.
Proper waste management is mandatory and involves several key stages:
- Segregation: Different types of waste, such as items saturated with liquid blood versus used needles (sharps), must be handled and containerized separately.
- Containment: All biohazardous materials must be placed in specially designed, leak-proof, puncture-resistant red bags or containers.
- Labeling: Every container must be clearly marked with the universal biohazard symbol, leaving no ambiguity about its contents.
- Disposal: This waste must be transported by a licensed biohazard waste hauler to a certified facility for treatment, typically via incineration or steam sterilization (autoclave).
Needlestick injuries remain a primary mode of transmission for bloodborne pathogens during waste handling. The stakes are incredibly high, considering hepatitis C affects an estimated 50 million people worldwide, and 39.9 million were living with HIV as of 2023. You can find more data on the prevalence of blood-borne diseases from trusted resources.
Knowing When to Call in the Pros
There is a clear distinction between a minor incident and a biohazard situation requiring professional intervention. While a single drop of blood on a sealed countertop may be manageable with the right PPE and disinfectant, certain scenarios are immediate indicators for professional help.
The moment a biohazard penetrates porous materials like carpet, drywall, wood, or grout, the situation changes entirely. Pathogens can migrate deep into these substrates, making surface cleaning ineffective and creating a hidden, long-term hazard.
It is time to call a professional biohazard remediation company for:
- Large spills of blood or bodily fluids
- Any contamination of porous materials
- Trauma and crime scenes
- Situations involving known infectious diseases
Attempting a major cleanup without certified training, specialized equipment, and a thorough knowledge of professional biohazard waste disposal protocols is unsafe and creates significant personal and legal risk. A certified company like 360 Hazardous Cleanup possesses the expertise to ensure a scene is not just visually clean, but biologically safe.
Got Questions About Bloodborne Pathogen Safety? We've Got Answers.
When facing bloodborne pathogens, uncertainty can be a significant source of stress. Getting clear, expert answers is crucial for making informed decisions, whether you are managing workplace safety or confronting an unexpected hazardous event.
Here, we address some of the most common questions our professional teams encounter.
What's The Difference Between Universal and Standard Precautions?
This is a key distinction that reflects the evolution of safety protocols in our industry.
Universal Precautions was the original framework, directing personnel to treat all human blood and certain body fluids as if infectious for pathogens like HIV and Hepatitis B.
Today, the industry gold standard is Standard Precautions. This is a more comprehensive and protective approach. It expands on the original concept, instructing us to treat all blood, all body fluids (except sweat), non-intact skin, and mucous membranes as potentially infectious, without exception. It is a broader, more rigorous mindset that applies to every situation, ensuring the highest level of safety.
Can I Just Use Bleach to Clean Up a Blood Spill?
This is a frequent question. While a 1:10 bleach-to-water solution has disinfectant properties, it is rarely the appropriate tool for biohazard remediation, and professionals avoid it for several reasons.
Bleach is highly corrosive and can cause permanent damage to surfaces. Its fumes are a significant respiratory irritant. Furthermore, its disinfecting efficacy degrades rapidly after being mixed and is compromised by the presence of organic material, requiring a thorough pre-cleaning step.
For anything more than a minuscule drop on a non-porous surface, bleach is inadequate. When blood has penetrated porous materials like carpet, wood, or drywall, it is completely ineffective. Certified technicians utilize stable, EPA-registered, tuberculocidal disinfectants that are engineered to eliminate dangerous pathogens without destroying property or creating secondary chemical hazards.
How Long Can Viruses Like HIV or Hepatitis Survive Outside the Body?
The environmental survivability of pathogens varies dramatically, which is precisely why every scene must be treated with the utmost caution.
- Hepatitis B (HBV) is exceptionally resilient. This virus can remain infectious in dried blood for a week or longer at room temperature.
- Hepatitis C (HCV) can also survive on surfaces for up to four days.
- HIV, in contrast, is very fragile and dies within hours once the fluid carrying it dries.
Because of the extreme hardiness of HBV, any dried bloodstain, regardless of its apparent age, must be treated as a potential biohazard. There is no room for assumption in this line of work.
When Is It Time to Call a Professional Biohazard Remediation Company?
The answer is straightforward: call a professional the moment a situation exceeds your training, equipment, or comfort level. Seeking expert help is the most responsible and safest course of action.
Specifically, a certified company is essential for the following scenarios:
- Trauma Scenes: Any situation involving an unattended death, suicide, or violent crime demands a highly specialized skill set, regulatory compliance, and a compassionate, professional approach.
- Large Spills: The larger the spill, the greater the risk of cross-contamination. Professionals have the containment procedures to manage this risk effectively.
- Porous Surface Contamination: Once blood has been absorbed by carpet, drywall, subflooring, or grout, it cannot be removed by surface cleaning. The contamination lies deep within the material and requires professional remediation.
- Known Infectious Diseases: If there is reason to believe the source individual had a communicable disease, engaging a professional is essential for safe containment and disposal.
A professional team operates under OSHA's stringent standards, possesses the correct PPE and disinfectants, and has the legal authority to properly transport and dispose of biohazardous waste. Choosing a certified provider protects you from physical harm, emotional trauma, and serious legal liability.
When you are faced with a situation that requires more than standard cleaning, you need a team that can restore certainty and safety to your environment. 360 Hazardous Cleanup provides expert biohazard remediation with an unwavering commitment to restoring your property and your peace of mind. If you need immediate, professional assistance, contact us 24/7.