The answer to whether urine is a biohazard is nuanced: it depends on the circumstances.
While urine from a healthy individual is predominantly sterile, this fact does not encompass the full spectrum of risk. The situation changes dramatically the moment specific factors are introduced—such as the presence of blood—transforming a simple cleanup into a regulated biohazard event that demands professional intervention.
Defining the Biohazard Potential of Urine
The critical question is not merely what the substance is, but what potential pathogens it may carry. A small spill in a private home presents a different level of risk than a significant volume in a public facility, healthcare setting, or at a trauma scene.
The defining characteristic of a biohazard is its potential to transmit infectious diseases. While urine is approximately 95% water, it can become a vector for dangerous pathogens when contaminated with other bodily fluids. For this reason, professional standards, particularly in commercial or healthcare environments, mandate treating all bodily fluids with the utmost caution, as the health status of the source is often unknown.
Key Factors That Change the Risk Level
Specific conditions can immediately escalate a urine spill from a routine cleaning task to a serious health threat. Recognizing these factors is the first step toward ensuring safety and regulatory compliance.
Here are the critical elements to assess:
- Presence of Blood: This is the most significant indicator of a biohazard. Even a microscopic amount of blood can carry bloodborne pathogens like HIV or Hepatitis B and C.
- Known Infections: If the source individual has a urinary tract infection (UTI), kidney infection, or another communicable disease, their urine contains harmful bacteria or viruses that can be transmitted.
- Large Volume: A substantial spill creates more than just a larger mess; it establishes a breeding ground for mold and bacteria, particularly if it saturates porous materials like carpet, subflooring, or drywall.
- Environmental Context: The location of the spill is paramount. A spill in a highly regulated environment such as a hospital, clinic, or daycare is managed with a much higher level of precaution than one in a private residence due to stringent compliance standards and public health obligations.
This flowchart illustrates the essential assessment process.
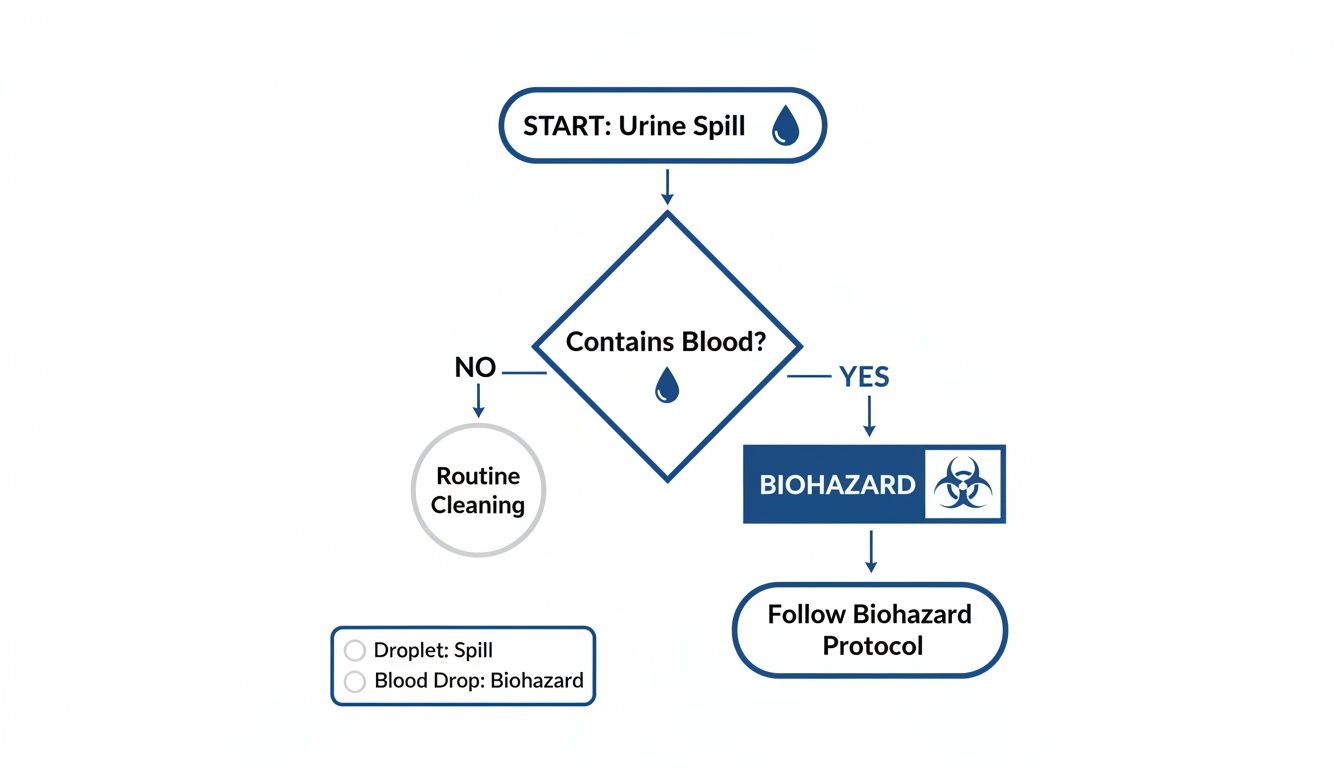
As the flowchart indicates, the presence of blood is the definitive factor that automatically classifies a urine spill as a biohazard requiring a professional, compliant response.
For clearer understanding, this reference table summarizes the risk levels associated with different scenarios.
Urine Biohazard Risk Assessment
| Scenario | Biohazard Risk Level | Primary Concern |
|---|---|---|
| Small spill, no blood, healthy individual | Low | Odor, staining |
| Urine from a person with a known UTI | Moderate | Bacteria (e.g., E. coli) |
| Large volume spill (e.g., saturated carpet) | Moderate to High | Mold, bacterial growth, structural damage |
| Any spill with visible blood | High | Bloodborne pathogens (HIV, Hepatitis B/C) |
This table demonstrates how rapidly the risk profile can escalate based on these critical details.
This authoritative stance is supported by health and safety experts. Research from Cornell University confirms that urine is generally not considered hazardous unless it contains visible blood or originates from an individual with a known infection. In such cases, it must be handled using universal precautions—the industry-mandated standard of treating all bodily fluids as potentially infectious.
It is impossible to identify invisible pathogens without professional training and equipment. For a comprehensive overview, you can explore our full guide to the biohazard risks of different bodily fluids.
When Normal Urine Becomes Hazardous Waste
While urine from a healthy person is mostly water, certain conditions can transform it from a simple mess into regulated hazardous waste. This occurs when urine becomes a vehicle for dangerous materials under specific circumstances.

Understanding this tipping point is not just about cleanliness; it is about mitigating genuine health risks. Three primary factors—the presence of blood, infectious diseases, and volume—escalate the danger level of what might otherwise seem like a minor spill.
The Contamination Factor of Blood
The single most critical factor that elevates urine to biohazard status is the presence of blood. The moment blood mixes with urine, the entire fluid must be treated as regulated medical waste according to OSHA standards. This is because blood can carry dangerous bloodborne pathogens.
These microorganisms cause serious, sometimes life-threatening, diseases, including:
- Hepatitis B Virus (HBV): A potent virus that attacks the liver, leading to acute and chronic illness.
- Hepatitis C Virus (HCV): Another viral infection causing chronic liver inflammation, which can result in severe long-term health complications.
- Human Immunodeficiency Virus (HIV): The virus that causes AIDS, a condition that compromises the immune system.
Because these pathogens are invisible to the naked eye, any urine containing visible blood is presumed to be infectious. This is why professional remediation is not only recommended but often legally mandated—it is the only way to ensure these unseen threats are completely neutralized.
When Illness Introduces Pathogens
Beyond blood contamination, the source individual's health is a significant factor. Urine can become a biohazard if the person has an active infection that sheds pathogens through their urinary system. A common example is a severe urinary tract infection (UTI), which can load urine with bacteria like E. coli.
Other kidney diseases and systemic infections can also release harmful microorganisms into the urine. If an individual comes into contact with this contaminated fluid—whether through a skin abrasion, inhalation of aerosolized droplets, or accidental ingestion—the illness can be transmitted. Immunocompromised individuals, the elderly, and young children are particularly vulnerable.
In public, commercial, or rental properties, the health status of the source is almost never known. For this reason, safety protocols demand that any significant bodily fluid spill be managed with extreme caution, assuming it is infectious until professionally proven otherwise.
The Dangers of Large Volumes
The final escalating factor is volume. While a small, contained puddle can typically be managed with standard cleaning protocols, large quantities of urine present a far more complex environmental health threat. This is frequently encountered in hoarding situations, cases of severe incontinence, or unattended death scenes.
When large volumes of urine saturate porous materials such as carpet, drywall, wood subflooring, or furniture, a dangerous chain reaction begins. First, uric acid begins to corrode and degrade these materials. Concurrently, the persistent moisture creates an ideal breeding ground for bacteria and mold.
This sustained dampness fuels exponential microbial growth, leading to a cascade of issues:
- Severe structural damage as wood rots and drywall deteriorates.
- Pervasive, noxious odors from bacterial off-gassing.
- Airborne contaminants, including mold spores and aerosolized bacteria, which can trigger respiratory problems and allergic reactions.
At this stage, the problem is no longer a simple stain but a widespread environmental hazard that has compromised the building’s structural integrity and indoor air quality. Understanding these complexities is vital for proper remediation, and you can learn more in our detailed guide on what qualifies as hazardous waste and its safe disposal.
Understanding OSHA and EPA Biohazard Regulations
When a spill becomes a potential biohazard, it transitions from a simple cleaning issue to a matter of federal and state regulation. For property owners and facility managers, understanding this legal framework is critical for ensuring public safety and compliance.In the United States, the Occupational Safety and Health Administration (OSHA) and the Environmental Protection Agency (EPA) establish the primary regulations. These are not mere guidelines but legally binding standards designed to protect workers, the public, and the environment from hazardous materials. Non-compliance can result in significant fines, legal liability, and, most importantly, severe health risks.
OSHA and the Bloodborne Pathogens Standard
The most important regulation concerning urine spills is OSHA's Bloodborne Pathogens Standard (29 CFR 1910.1030). This standard is the foundation of workplace biohazard safety. While it does not explicitly name urine, it contains a critical clause that applies the moment blood is present.
The standard governs "other potentially infectious materials" (OPIM), defined as any bodily fluid visibly contaminated with blood. If a urine spill contains even a trace of visible blood, it automatically falls under OSHA’s strictest regulations.
Key Takeaway: The presence of blood is the legal trigger. Once urine is mixed with blood, it is classified as regulated medical waste and must be handled according to federal law, which mandates specific personal protective equipment (PPE), decontamination procedures, and disposal protocols.
This distinction is paramount. It means an employer cannot simply ask an employee to clean the spill without providing proper training and certified protective gear. The first step in managing these risks is conducting a thorough infection control risk assessment to ensure your facility is prepared and compliant.
EPA Guidelines and Waste Disposal
While OSHA's role is to protect workers during the cleanup process, the EPA regulates the final, critical step: proper disposal. The EPA’s regulations for medical waste—often enforced at the state level—are designed to prevent biohazardous materials from contaminating the environment or harming public health.
Materials contaminated with blood-tinged urine cannot be discarded in standard trash. They must be:
- Segregated: Placed in specialized, leak-proof, and clearly labeled biohazard containers.
- Transported: Handled exclusively by licensed and certified biohazard waste carriers.
- Treated: Transported to a specialized facility for disposal, typically through incineration or autoclaving, which renders pathogens harmless.
Failure to adhere to these disposal protocols can result in severe penalties. This is another reason why engaging a professional remediation company like 360 Hazardous Cleanup is essential—we manage the entire process from start to finish, ensuring full compliance with all regulations. For a deeper understanding of these requirements, please see our guide on OSHA and biohazard cleanup compliance.
The scale of this issue is larger than most people realize. Globally, 15% of all waste from healthcare facilities is considered hazardous. In developed countries, hospitals can generate up to 11 kg of this waste per bed, every single day. This data underscores the critical importance of these regulations for protecting our communities.
The Hidden Dangers of Improper Cleanup
Mistaking a biohazard spill for a simple stain or odor is a significant error. Attempting to clean it without understanding the associated risks is akin to painting over rust—it conceals the problem without resolving the underlying damage. The consequences can be severe, impacting health, property value, and legal standing.

The dangers extend beyond unpleasant odors to include immediate health threats, long-term structural damage, and serious legal liability. Recognizing how these risks are interconnected makes it clear why professional remediation is an investment in safety.
Immediate Health Risks from Unseen Pathogens
The most immediate threat from an improper cleanup is exposure to invisible pathogens. If urine contains blood or comes from an individual with an infection, it can serve as a delivery system for microorganisms. Standard household cleaners lack the efficacy to eradicate these resilient bacteria and viruses.
Without proper Personal Protective Equipment (PPE) and containment protocols, these germs can easily be spread. They can become airborne during scrubbing, be transferred to other surfaces, or enter the body through a small cut. This puts family members, employees, or tenants at risk of infection.
A surface may appear clean, but this can provide a false sense of security. The true danger is microscopic. Pathogens can survive for days or weeks if not neutralized with professional-grade disinfectants and proven remediation techniques.
This is a more significant issue than many realize. The market for urine collection devices is projected to reach USD 4.57 billion by 2032, partly because nearly 200 million people worldwide manage urinary incontinence. As the population ages, these types of spills will become more common, making proper biohazard protocols more critical than ever.
Long-Term Structural and Financial Damage
Beyond immediate health risks, the chemical properties of urine slowly cause property damage. Uric acid is corrosive and, over time, can erode floor finishes, weaken wood, and tarnish metal. The most significant destruction, however, occurs when moisture penetrates below the surface.
Once urine saturates porous materials like carpet padding, subflooring, or drywall, it creates a pocket of moisture that rarely dries completely. This becomes an ideal environment for mold and bacteria, initiating a chain reaction of costly problems:
- Wood Rot: Persistent moisture compromises the structural integrity of floors and support joists.
- Drywall Degradation: Saturated drywall softens, crumbles, and loses its structural capacity.
- Pervasive Odors: As bacteria break down urea, they release ammonia gas, the source of the foul, persistent odor that is nearly impossible to eliminate without professional intervention.
- Permanent Staining: Pigments in urine can cause permanent stains on wood, tile grout, and fabrics.
What begins as a single incident can quietly escalate into thousands of dollars in repairs, often requiring the removal and replacement of entire sections of floors, walls, and insulation.
Legal and Financial Liability
For business owners, landlords, and property managers, the stakes are even higher. Failure to properly remediate a biohazard scene—which can include a significant urine spill—exposes you to considerable legal and financial risk. If an employee or tenant becomes ill from exposure, you could face negligence lawsuits and workers' compensation claims.
Furthermore, non-compliance with OSHA and EPA regulations for handling biohazardous waste can lead to substantial fines. If an improper cleanup is performed, an insurance carrier may deny the claim, leaving you responsible for all remediation and repair costs. Professional cleanup is not just about cleanliness; it is about documenting a compliant, safe process that protects you from future liability. You can learn more about these consequences in our guide on what happens if you don't properly clean a biohazard scene.
When to Call a Professional for Cleanup
Distinguishing between a simple mess and a true biohazard can be challenging, particularly during a stressful or traumatic event. While some small spills can be managed with standard cleaning supplies, certain situations present risks far too serious for anyone but a trained and certified professional. These scenarios demand specialized equipment, strict regulatory compliance, and a thorough understanding of how to eliminate invisible threats.
Attempting to clean a high-risk scene yourself can lead to dangerous pathogen exposure, cause irreversible property damage, and result in legal complications. Making the correct decision protects your health and provides the assurance that the environment has been fully restored to a safe, habitable condition.
Scenarios Demanding Immediate Professional Help
Certain events create biohazard risks that are too complex and dangerous to be addressed with standard cleaning products. If you encounter any of the following situations, your first action should be to contact a certified remediation company like 360 Hazardous Cleanup. These are clear indicators that professional expertise is required.
Key triggers for professional intervention include:
- Trauma or Crime Scenes: Any location where an injury, violent crime, or serious accident has occurred requires professional remediation. Bodily fluids, including urine potentially mixed with blood, are often present and carry a high risk of bloodborne pathogen transmission.
- Unattended Death: Following an undiscovered death, the natural decomposition process releases widespread biohazardous materials. These scenes are extremely hazardous and require specialized techniques to render the area safe.
- Hoarding Environments: Severe hoarding situations are frequently contaminated with human or animal waste. When large volumes of urine saturate flooring, walls, and personal belongings, a dangerous breeding ground for bacteria, viruses, and mold is created.
- Large-Scale Spills in Commercial Facilities: A significant spill in a public space—such as a nursing home, office building, or daycare—mandates a professional response. This is necessary to comply with OSHA regulations and protect employees, customers, and residents.
- When the Source's Health Status Is Unknown: In a public or rental property setting, it is impossible to know if the involved individual had an infectious disease. Professionals operate under the principle of universal precautions, treating all bodily fluids as potentially infectious. This is the only method to guarantee safety for everyone.
For a deeper analysis of these situations, our guide provides more detail on when biohazard cleaning is needed, so you can feel fully informed.
The Value of a Certified Remediation Team
Engaging a professional biohazard team offers far more than just cleaning services. During an emotional and challenging time, it provides a structured, safe, and compassionate solution that manages every detail, alleviating the burden from you.
A professional remediation service is an investment in certainty. It provides assurance that every microscopic threat has been neutralized, all regulations have been met, and the space is truly safe for occupancy again. This peace of mind is invaluable during a high-stress event.
A certified team delivers critical advantages that a DIY approach cannot replicate. We begin with a thorough assessment to identify all contaminated areas, including those hidden beneath floors or within walls. We utilize industrial-grade, EPA-registered disinfectants that eliminate pathogens resistant to household cleaners.
Finally, we ensure all biohazardous waste is properly collected, transported, and disposed of in accordance with strict federal and state laws. This process provides you with the necessary documentation to protect you from future liability. It is a comprehensive approach that ensures the property is not just superficially clean but holistically safe and restored.
Frequently Asked Questions
Even with an understanding of the risks, real-world cleanup situations can generate specific questions. Obtaining clear, factual answers is essential for making safe and confident decisions during stressful times. Here are the most common questions our experts receive, with direct and authoritative answers.
Can the Smell of Urine Be Hazardous to My Health?
While the odor of urine itself is not toxic, a strong, persistent ammonia smell is a critical warning sign that should not be ignored. This sharp odor indicates that bacteria are actively breaking down urea in a large or long-standing spill.
An environment with such a strong smell is an ideal breeding ground for mold and harmful microbes. High concentrations of ammonia gas can irritate the eyes, throat, and lungs, particularly for individuals with asthma or other respiratory sensitivities.
More importantly, the odor is a symptom of an underlying biohazard. The primary health risk comes from inhaling airborne mold spores and bacteria thriving in the contaminated area. The smell signals a deeper problem that requires professional remediation to locate and eliminate the source, not merely mask the odor.
Is Animal Urine Considered a Biohazard?
Yes, absolutely. Animal urine can often pose a greater risk than human urine. Urine from pets, and particularly from pests like rats and mice, can transmit numerous serious zoonotic diseases—illnesses that spread from animals to humans.
Some of the major diseases linked to animal urine include:
- Leptospirosis: A severe bacterial infection that can lead to kidney damage, meningitis, liver failure, and death. It is transmitted through contact with urine from infected animals.
- Hantavirus: A severe and sometimes fatal respiratory illness transmitted through the urine, droppings, and saliva of infected rodents.
- Salmonellosis: While often associated with feces, bacteria like Salmonella can contaminate any environment where pests are present.
As with human urine, the danger multiplies with the volume and duration of contamination. Situations involving animal hoarding or severe infestations create widespread hazards that saturate building materials and degrade air quality, demanding professional biohazard cleanup to neutralize all pathogens and restore the property to a safe condition.
What Is the Difference Between Cleaning and Remediation?
This is a critical distinction. While the terms may sound similar, they represent fundamentally different processes and outcomes. Standard cleaning addresses visible dirt, whereas biohazard remediation eliminates microscopic threats.
Standard Cleaning
- Goal: To remove visible dirt and grime from a surface.
- Tools: Standard household products such as soap, detergents, and all-purpose disinfectants.
- Scope: A surface-level activity that does not address contamination that has penetrated porous materials like wood, drywall, or carpet padding.
Biohazard Remediation
- Goal: To return an environment to a verifiably safe, habitable state by eliminating all biological and chemical contaminants.
- Tools: Specialized equipment, comprehensive PPE, and EPA-registered, hospital-grade disinfectants designed to kill resilient pathogens.
- Scope: A comprehensive, scientific process governed by strict OSHA protocols. It involves site containment, removal of contaminated materials (including subflooring or drywall), disinfection of all remaining surfaces, and the use of technologies like ozone treatments to eliminate odors at their source.
Simply cleaning an area that requires remediation leaves behind hidden dangers and creates a false sense of security while allowing pathogens and mold to continue growing unseen.
Does Homeowners Insurance Cover Urine Damage Cleanup?
Whether homeowners insurance covers urine damage cleanup depends on the specific policy and, crucially, the root cause of the damage. Coverage typically hinges on whether the incident was "sudden and accidental" as opposed to a gradual or maintenance-related issue.
Biohazard remediation is more likely to be covered if it is linked to a covered peril, such as a trauma, crime scene, or accidental death on the property. These are generally considered unforeseen events.
However, damage resulting from long-term issues is almost always excluded. For instance, contamination from years of pet urination, a hoarding situation, or deferred maintenance will likely be classified as a preventable problem, leading to a denial of the claim. It is essential to review your policy's "perils" and "exclusions" sections carefully.
Navigating an insurance claim during a crisis can be overwhelming. As experienced professionals, we regularly work directly with insurance carriers. We can assist you in documenting the damage correctly, interpreting your policy, and managing the claims process to optimize your chance for coverage.
In times of crisis and uncertainty, you need a partner who provides not just expert cleanup, but also compassion, discretion, and peace of mind. The team at 360 Hazardous Cleanup is available 24/7 to restore safety to your property and help you move forward. For immediate, professional assistance, visit us at https://360haz.com.